What I Learned from Carol’s COPD Journey: We Can Do Better
NuvoAir CEO Lorenzo Consoli reflects on his time with Carol, a NuvoAir patient, and her experience living with COPD.
At NuvoAir, our first company value is being patient-obsessed. This reminds us every day that we are here to support people living with difficult health conditions. It’s our North star, the reason why most of us joined a mission-driven organization, and the glue that brings our team together across two continents.
Meeting Carol
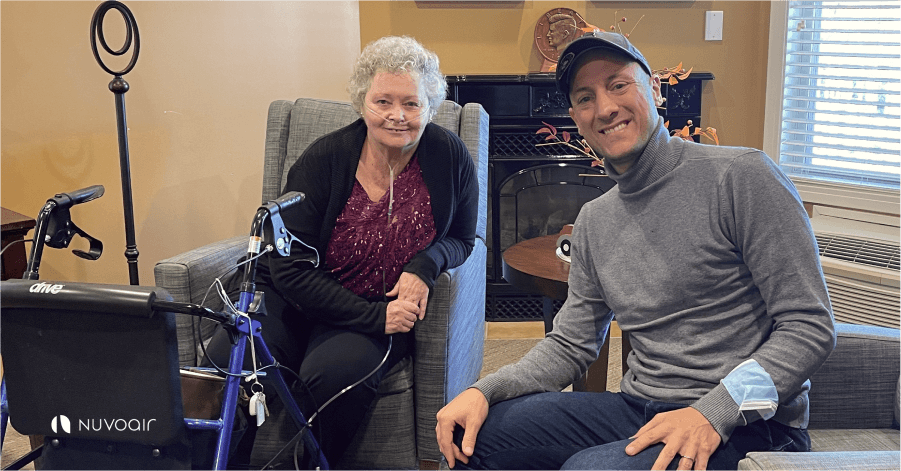
Each week our team shares incredible stories from the patients we serve and the innovative health plans and partners we work with to improve care of those in need. One of the people I’ve had the pleasure of meeting is Carol, a 70 year old woman living with chronic obstructive pulmonary disease (COPD). I spent two hours with Carol in her nursing facility in Massachusetts, not far from our office in Boston. Meeting Carol made me reflect on the state of COPD in the U.S., the healthcare system in general, and what we can do to make it better.
I met Carol on a mild autumn day in November, and on my way, I bought her a plant. She was waiting for me in the library of the facility and welcomed me with a warm smile that grew warmer when she realized the plant was a gift for her.
It quickly became an emotional conversation, which I was barely prepared to handle. She told me that she was the first of four siblings, and was forced to grow up very quickly. Having lost her mother when she was a young child and her father just a few years later, it was not an easy childhood to say the least.
Despite a tough life, Carol’s energy was explosive. Her eyes were intense, and she had a sparkling sense of humor. She did not spare details when asked to recall difficult memories.
Hospitalizations and rehab
She told me that she was a heavy smoker and a drinker early in her life. Her lungs were very prone to pneumonia, but the smoking and the weather of Florida, with its heavy humidity, did not help. She exacerbated often and in her mid-40s, found herself hospitalized for over a year with difficult-to-treat pneumonia. It was during this incident that she was diagnosed with COPD.
After a year in the hospital, she was transferred to a rehab program. She recalled how difficult those days were for her. The rehab program stripped away her individuality, but she learned more about herself and her condition.
Carol shared that the process of getting the right medicine was not easy. Doctors began the painstaking journey of matching her symptoms to the right inhalers — ones that were the most effective with the least side effects. After months of trial and error, she got on the right therapies. She is currently on Montelukast and a long-acting muscarinic antagonist (LAMA) inhaler and has been using these medications for over ten years. But, as she recounted with a smile, her adherence was far from optimal in the early days.
When she left rehab, a visiting nurse came to her home weekly to perform check-ups. Carol said she never really connected with her, mostly because she felt as though she was following a script rather than truly engaging and caring about her. Had this nurse shown more empathy, Carol admits, she may have stuck to the nurse’s prescribed exercises far more than she did.
Losing hope
Over the years, her lungs got worse, and so did her dyspnea, her difficulty in breathing. Daily activities became more difficult to perform. She explained how simple things such as making the bed, taking a shower, or buying groceries became too hard. She was constantly tired and slept all day. Over time, she started to restrict her possibilities in life, and was left with little hope. Carol had thought that this was the beginning of the end. After all, her parents died when they were young, perhaps it was her time as well, she remembered with a trembling voice.
The hard truth was that her blood oxygen level had dropped dangerously into the low 80’s, which was discovered by a respiratory therapist at one of Carol’s rare visits to the doctor. She was immediately prescribed oxygen and, from that moment, a big oxygen tank became her closest companion. This was a major turning point in Carol’s life. When she started oxygen therapy, she could finally breathe again and return to a more normal life.
By that time, she had moved in with her cousin, and Carol could support her with day-to-day activities and chores. Helping her cousin was very important to her, and being able to contribute again gave her a sense of purpose. Carol didn’t mind bringing her oxygen tank everywhere, and while other COPD patients felt the stigma of carrying around a huge medical device, she did not, though she admits it wasn’t always easy. About two years ago she moved into her current nursing home, thanks to the Medicare PACE program. She wasn't happy at first with the change and unfamiliarity, but now she has her routine, and she feels loved and cared for. Before moving to the nursing facility, she didn’t often attend her doctor appointments, but now she doesn’t miss even one. She feels she has a community around to support her.
Falling through the cracks
Carol’s difficult healthcare journey with COPD is common for millions of Americans. For patients with complex diseases like COPD, help often comes too late. The fragmented healthcare system fails to prevent people from falling through the cracks. A system that lacks coordination and empathy, and fundamentally fails to put patients at the center, is causing almost a million COPD hospitalizations each year — many of which could be prevented. This leads patients and their conditions to spiral and many lose hope due to devastating effects.
Perhaps Carol was diagnosed and appropriately treated too late. Currently, 16 million Americans are living with COPD and at least another 15 million are undiagnosed. This is clearly not acceptable. For the most part, Carol had to learn how to manage her COPD independently over the years. She explained that she was incorrectly using the nasal cannula of her oxygen for a long time. She was unsure of how to use her inhalers and clean her CPAP mask. There was no one around to support her when she had a doubt or a question and she did not trust her doctors as she felt they did not listen to her. As a result, she was prescribed oxygen only after years of living a heavily restricted life. She went through several smoking cessation programs with limited success, until nicotine gum finally worked for her.
Carol’s story leaves me with many questions. Could this whole process have been more optimal? Could there have been a more cohesive COPD management strategy to support Carol? Who does not believe so?
More importantly, Carol’s journey tells me that the system failed to truly see her, listen to her and deeply engage her. When I asked her if she could go back in time and change one thing about her healthcare experience, she replied without hesitation,
“I would have liked it if someone had truly understood me and taught me the importance of loving myself. Even with debilitating conditions, such as COPD, life must be about what we CAN do, not what we cannot.”
Carol was always reminded about what she could not do. This approach has profound implications because it leads patients to close themselves down and disengage with their health and the healthcare system.
It was 11:45 am and she was ready for lunch. It was time to go. I thanked her deeply for her time and left the nursing facility knowing that there is a lot of work to do to fix the current healthcare system — though no one player can do it alone. I was reassured that at NuvoAir, we are working on things that matter and together with dedicated partners, can improve the lives of millions of people living with COPD, like Carol, around the globe.